How to Accommodate Vision in Children and Youth with Bardet-Biedl Syndrome
This paper summarizes certain key vision-related needs of children and youth with Bardet-Biedl syndrome (BBS). It is intended as a utilitarian resource for parents, educators, vision care specialists, and psychologists, whose collaborative efforts are needed to develop a customized Individual Education Plan (IEP) for a student with BBS. It is not intended as a comprehensive report on the pathophysiology of vision compromise in BBS.
BBS is a rare genetic disorder that affects many body systems. Nearly all individuals with BBS have some impairment of vision. This is due to retinal degeneration. The degeneration typically causes subtle difficulties with vision in early childhood, followed by gradually worsening vision to the level of legal blindness in adulthood, although many exceptions to this typical course have been documented.
The retina is a multi-layered film that lines the inside of the eye and receives the light coming into the eye (see Figures 1 and 2). Light-sensitive photoreceptor cells in the retina, known as rods and cones, convert the light into a signal to neurons and thus start the process of seeing. In BBS, the rods and cones slowly degenerate and their ability to turn light into a signal is compromised.
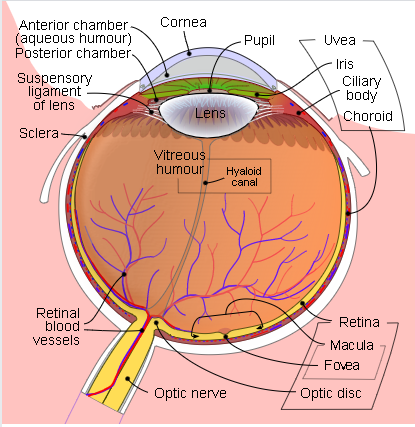
Figure 1. From Wikipedia, licensed under the Creative Commons Attribution-Share Alike 3.0 Unported license; Credit: Rhcastilhos and Jmarchn, 2007.
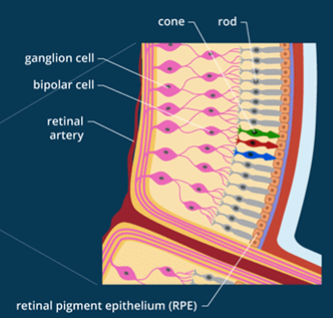
Figure 2. Detail of the retina.
Cones operate in daylight. Color vision depends on the cones, which are found all over the retina. Within the central retinal region, called the macula, cones are spaced very closely together in the fovea (a small indentation at the back of the eye) so that tiny, precise details can be seen. Some individuals with BBS lose cones and macular function early in the course of their retinal degeneration.
Rods operate in dim light. The rods are found all over the retina except at the very center. Off to the side, in a ring around the macula (rod ring), the rods are tightly packed. In low light, vision is normally best off to the side (peripherally). Some individuals with BBS lose rods and their peripheral visual field while maintaining quite good central vision.
Characterization of the status of the retina and vision provides information for planning services and educational programs for BBS students. Ophthalmologists and optometrists with expertise in pediatric low vision must perform these evaluations, the elements of which include:
- measurement of acuity using age/ability appropriate tests
- measurement of refractive error and correction (glasses) if indicated
- assessment of the visual field (often a manual test is more satisfactory than automated perimetry)
- appearance of the retina with photographic documentation
- optical coherence tomography (OCT) images of the macula (to evaluate retinal structure of the central part of the retina)
- measurement of the dark-adapted visual threshold, to assess “night vision”
- electroretinography (ERG), which is the only test that can assess function of all of the cones and rods in the retina.
Serial assessments of the student’s retina and vision are important because of the developing capabilities of the individual with BBS and because of the progressive nature of the BBS retinal disorder. Communication of the results of these assessments by eye care providers is ideally an interactive process involving all stakeholders—the individual with BBS, family, educators, and providers of community-based services.
Special Education for BBS
An IEP for a BBS student typically has several components. Creation of an IEP is a team effort, potentially involving special education administrators, public education school administrators, classroom teachers, teachers of the visually impaired (TVIs), school psychologists, and parents. Once a TVI has performed a thorough assessment, s/he, the classroom teacher, and/or the special education administrator must collaborate. A good IEP depends on the team’s ability to identify the strengths and weaknesses in the individual with BBS and is typically updated annually.
The BBS retinal disorder may lead to deficits in distance and near vision, visual field constriction, night-blindness, and disruption in color vision that may vary with lighting conditions, environmental factors, and attention—all of which may vary from day to day. As the retinal disorder progresses, visual abilities may also decline over time. Ideally, a TVI will perform a functional vision assessment annually, and at a minimum, every three years at a triennial IEP.
Teachers and paraprofessionals should be aware of visual symptoms and other manifestations of the syndrome. Visual fatigue and eye strain are the major complaints from students with low vision. Visual field deficits make it difficult to locate and focus on printed material.
Technology is rapidly advancing to enable the visually impaired or non-sighted BBS student to be educated alongside sighted peers in a public education setting. A good IEP should include a technology assessment that addresses the acquisition of adaptive vision technology and software, including computers/laptops/notebook.
Following are common recommendations that are often included in the IEP:
Classroom
- Offer BBS students more visual breaks than their classmates, to relieve fatigue.
- Preferential seating is recommended; the student should be seated closest to the teacher and the white board.
- Ensure good classroom lighting, which provides improved contrast on all printed materials. This can compensate for difficulty with vision in dim light and reduced contrast sensitivity.
- Use of a template, a place-marker, and reducing the amount of information per page may improve overall performance.
- Offer accommodations for academic testing to ensure equity, including extended time, audio-taped responses, and/or large print.
- Consider using Braille for the student.
Reinforce the use of eyeglasses and/or reading glasses, as recommended by the eye care specialist.

Adaptive Aids and Assistive Technology
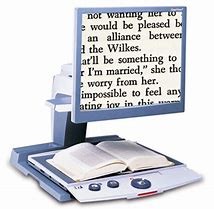
- Videomagnifiers, handheld portable electronic magnifiers, and telescopic devices should be considered.
- Consider other accommodations, such as appropriate software and/or apps that allow the student to access the curriculum.
- Advocate for the latest in computer technology. This may involve a large monitor and audio read-back software capability that enlarges print and can provide an auditory format for learning. (The audio description should complement the written text, including from large print.)
- Smart phones with text-to-speech and speech-to-text applications specific to the student’s unique needs are recommended.
- Low-tech aids, including hand-held magnifiers, large print lined paper, black felt tip pens, and optimal lighting should be considered.
- Tape recordings of educational activities such as lectures and instructional materials enable the BBS student to review the content at a later time.
- The student should receive a hard (or Braille) copy of overhead projection material prior to the lecture.
Orientation and Mobility (O&M)
- BBS youth need a certified O&M specialist to provide instruction on safe and independent travel at school, home, and in the community. As vision declines, training on use of a white cane as a tool for safe travel becomes essential. The cane also alerts the otherwise unaware sighted person to the visual impairment, a proven safety factor. Additional compensatory techniques taught by the O&M specialist are sensory development and use of the senses in combination with spatial awareness, self-protective, problem-solving, and human guide techniques to move safely through indoor and outdoor environments. Use of landmarks and compass directions along with cellphone accessible geo-map direction instructions should be taught.
- Many individuals with BBS have poor balance and orthopedic concerns, such as scoliosis, hip dysplasia, and leg length discrepancy. The O&M specialist should be aware of specialized individual needs and limitations.
Daily Living Skills
- Age-appropriate skills that may be required by the BBS student for independent living are usually taught as part of the classroom curriculum with the assistance of a TVI or Occupational Therapist. Such skills include hygiene, dressing, organization of school work, time management, household chores, and basic cooking and meal preparation.
Physical Education
- Adaptive physical education is essential to mitigate any poor coordination and clumsiness in addition to visual deficits. Low vision and loss of peripheral vision makes participation in fast-paced team sports difficult and increases risk of accidental injury. Alternative physical activities, such as swimming, weight training, and track/jogging, should be considered.
Communication
- Speech, language, and pragmatic (social) challenges are frequently present in individuals with BBS. Articulation differences are common. Mastering of speech sounds varies across this population. Conversations regarding continued targeting of speech sounds versus use of alternative communication supports are needed. An early focus on developing non-sighted skills is important for supporting the student’s comprehension skills in the longterm. Impaired social language skills (e.g., initiating interactions, reciprocity in conversations, perspective taking) are often present. Direct intervention in individual as well as group settings should be considered for the student’s future endeavors as well as fostering friendships with their peers.
Social
- Making friends can be very difficult for an individual with BBS. Deficits in social pragmatics amplified by vision deficits and social immaturity jeopardize the building of personal relationships and increase the chances of social isolation and bullying. Enabling visually impaired and non-sighted students to socialize with each other in a special education, teacher-led resource room setting can be critically important to developing maturity and building friendships and is strongly encouraged.
Transition IEP
- The goal of the transition IEP is to enable the student with BBS to be successful in whatever plans s/he wants to pursue after high school. Planning for transition into higher education (university, technical colleges) or vocational training is essential and should begin when the student is 16 years of age or younger. The transition IEP may include a variety of services including:
- Special classes or training
- Community-based experiences
- Information about available sources of post-high school help
- Expanded orientation and mobility training
- Training in living independently
- Outside services, including public and private vocational rehabilitation agencies, college guidance officers, and aging and disability services may need to play an active role in transition IEP development.
- As appropriate, the parent/care provider should be encouraged to assess whether or not there will be a need to secure legal guardianship once the child becomes an adult. Referral for legal services and appropriate neurology and/or neuropsychological testing by 17 ½ years of age is strongly encouraged. Advance Care Planning is recommended for those children who will not require a Guardianship once they become adults.
_____________
Robert Haws, MD, is a pediatric nephrologist and Director of the Marshfield Clinic Center of Excellence for BBS. Robie Jo Linn, CCC-SLP, is a speech pathologist at the Marshfield Clinic Health System, Rebecca E. Stewart, MA, is a retired vision specialist in the Santa Clara Unified School District, a Special Educator, and a BBS parent. Anna Maria Baglieri, OD, is an Instructor of Ophthalmology at Harvard Medical School (HMS) and a low vision clinician. Kathryn B. Miller, OD, is an Assistant Professor of Ophthalmology at HMS and a clinician/researcher in low vision and vision therapy. Anne B. Fulton, MD, is a Professor of Ophthalmology at HMS, Director of Medical Retina Service at Boston Children’s Hospital, a world-renowned researcher on function and structure of the developing eye, and a longtime physician whose patients are children with complex problems (congenital and acquired) of the visual system.
